Drug Use and Mental Illness

A mental illness may make a person more likely to use drugs—for example, for short-term relief from their symptoms—while other people may have drug problems that trigger the first symptoms of mental illness. Some drugs cause drug-induced psychosis, which usually passes after a few days. However, if someone has a predisposition to a psychotic illness such as schizophrenia, the use of illicit drugs may trigger the first episode in what can be a lifelong mental illness. The use of drugs can interact with mental illness in ways that create serious adverse effects on many areas of functioning, including work, relationships, health and safety.
It is important to note that, by themselves, these findings do not establish a causal link between mental illness and drug use—the mental illness may have preceded the drug use or vice versa.
In addition to asking people if they have been diagnosed or treated for a mental illness in the previous 12 months, the survey also includes the Kessler 10 scale (K10), which was developed for screening populations for psychological distress.
Since the 2010 survey, the proportion of adults who had been diagnosed with or treated for a mental health condition in the previous 12 months has been increasing and increased again between 2016 and 2019 (from 12.0% in 2010 to 15.9% in 2016 and to 16.9% in 2019). Increasing literacy and awareness around mental illness in Australia may partially explain these reported increases (National Mental Health Commission of NSW 2015), however, there are likely to be other factors involved including changing trends and patterns in the use of alcohol and other drugs.
Are levels of psychological distress increasing?
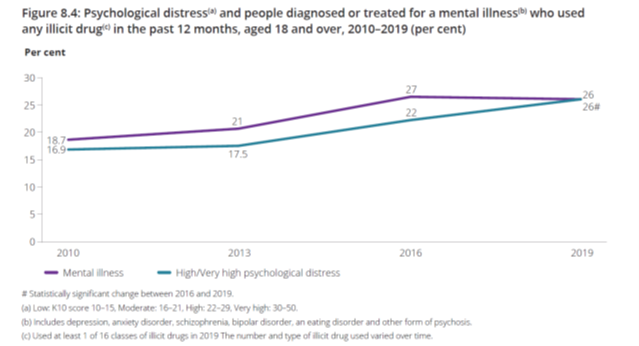
In 2019, the proportion of adults who reported high or very high levels of psychological distress increased (11.7% in 2016 compared with 14.0% in 2019) (Table 8.5). This increase occurred among adults who had used an illicit drug in the previous 12 months (22% in 2016 compared with 26% in 2019) and those who had not used an illicit drug (9.7% compared with 11.7%). The increase in high or very high psychological distress levels was most noticeable among people who had used cannabis in the last 12 months (24% in 2016 compared with 28% in 2019).
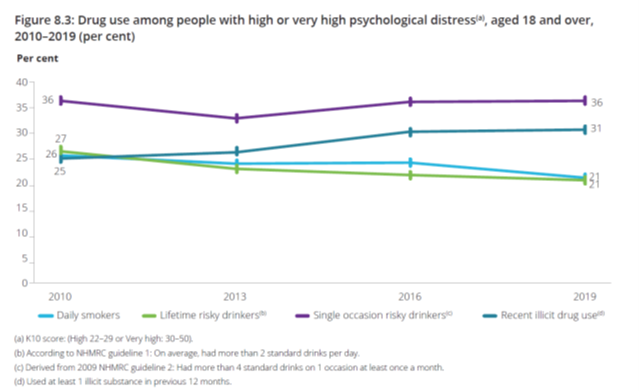
Among adults with high or very high levels of psychological distress, the proportion smoking daily was stable between 2010 and 2016 but declined in the most recent 3-year period (from 24% to 21%). Since 2010, the proportion exceeding the lifetime risk guideline to reduce the harm from alcohol has declined (from 27% to 21%) but the proportion exceeding the single occasion risk guideline was similar between 2010 and 2019 (Figure 8.3). The proportion who had used any illicit drug in the previous 12 months increased (from 25% in 2010 to 31% in 2019).
(Page 68).
Drug use among people diagnosed or treated for a mental health condition
Among people who recently used illicit drugs aged 18 and over, the proportion who had been diagnosed with or treated for a mental health condition in the previous 12 months remained stable over the most recent 3-year period at 26%, but has increased since 2010 (from 18.7%; Figure 8.4).
Although the proportion smoking daily declined between 2016 and 2019, no clear trend since 2010 is evident. However, the proportion is consistently higher than for people who have not been diagnosed or treated for a mental illness.
(Page 68).
(Page 69).
Drug use still higher among people with a mental illness or high psychological distress
Since 2010, people who had used an illicit drug in the previous 12 months have been at least twice as likely as people who have not used an illicit drug to experience high or very high levels of psychological distress in the 4 weeks before completing the survey (Table 8.6). High levels of psychological distress is consistently greater among people who report meth/amphetamine use in the previous 12 months.
In 2019, compared with people who had not been diagnosed or treated for a mental health condition in the previous 12 months, people with a mental health condition were:
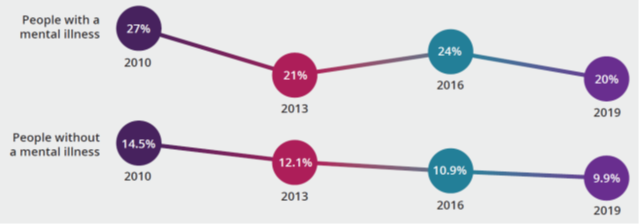
- twice as likely to smoke daily (20% compared with 9.9%)
- about 1.2 times as likely to drink alcohol at levels that exceed the lifetime risk (21% compared with 17.1%) and single occasion risk guidelines (at least monthly) (31% compared with 25%)
- 1.7 times as likely to have recently used any illicit drug (26% compared with 15.2%)
- about 2.2 times as likely to have used meth/amphetamine (2.6% compared with 1.2%)
- 2.1 times as likely to use pharmaceuticals for non-medical purposes (7.6% compared with 3.6%)
Reference: Australian Institute of Health and Welfare. (2020). National Drug Strategy Household Survey 2019. Drug Statistics series no. 32. PHE 270. Canberra AIHW. Pages 67 – 69.