Snapshots of Illicit Drug Use in Australia – 2019
Cannabis
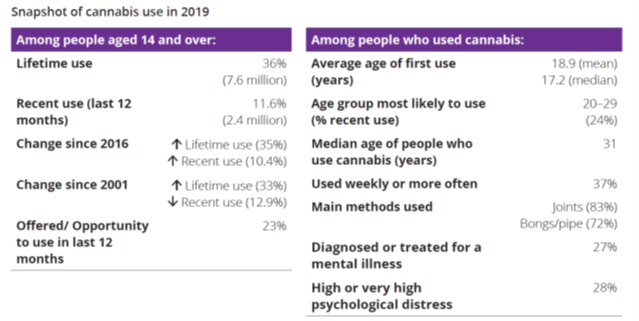
(Page 34).
Cocaine
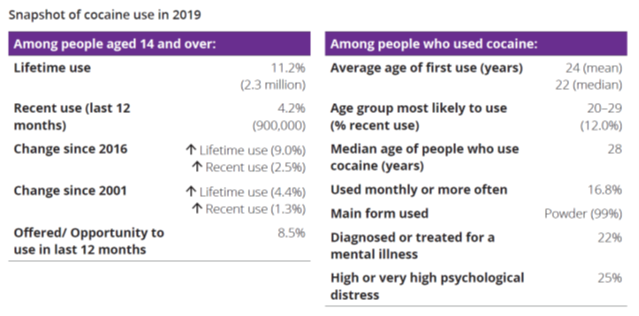
(Page 36).
Ecstasy
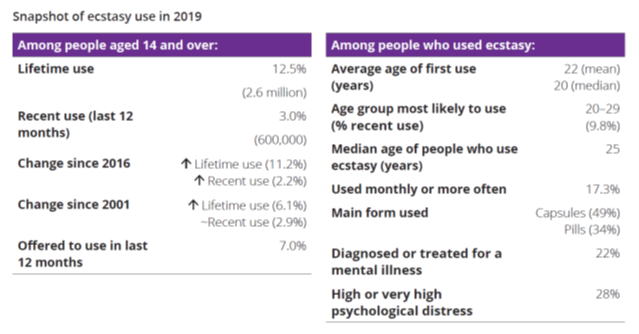
(Page 38).
Methamphetamine
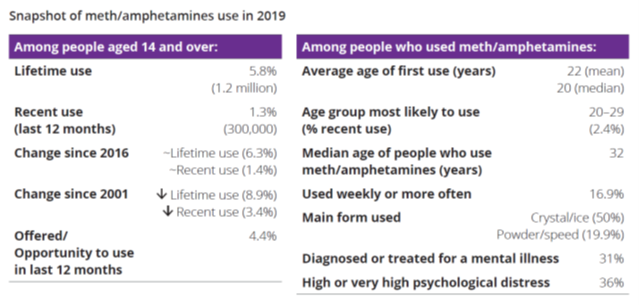
(Page 39).
Reference: Australian Institute of Health and Welfare 2020. National Drug Strategy Household Survey 2019. Drug Statistics series no. 32. PHE 270. Canberra AIHW. Pages 34 – 39.
The Comorbidity Roundabout
The top causes of disease burden among Australians are dominated by mental health and alcohol or other drug use (AOD) disorders. Of significant concern is the common co-occurrence (i.e. comorbidity) of mental health and AOD disorders. It is estimated that almost one in five Australians with a mental health disorder also have a co-occurring AOD disorder.
Conversely, between 47-100 per cent of people in AOD treatment in Australia have co-occurring mental health disorders. This common comorbidity remains a major cause of disability, poor quality of life, early mortality and poses a significant challenge for the Australian health system. Despite growing evidence about integrated treatment, people with mental health and alcohol or another drug use comorbidity can find themselves on a ‘comorbidity roundabout’.
This study collated the perspectives of people with lived experience of these issues to better understand how mental health and AOD services can better address their experiences and treatment needs.
“I find that I use alcohol to escape feeling the fear and loss of control over my own mind. When I’m drunk it’s almost like I have a rest and my brain recovers and I can be again safe at my grandma’s place without a worry in the world. I would be loved again and I would be worth something not just the scraps of who I used to be.”
“Often people use drugs to relieve their mental health problems or memories of trauma. They are isolated and scared. Everyone wants to be included in life.”
“People thinking that I’m weak for taking medications, family thinking that all I need is a job, or to do something better, or that I have caused it myself, or that I just need to get over what happened to me and to stop playing the victim.”
“Providing education through visual means to the community regarding the causes and triggers for these issues and the struggles faced by individuals living with mental health and or AOD issues is crucial. Using all available channels such as social media, radio and television so that people are more understanding and equipped to better handle situations where a friend or loved one may need help and support.”
“Empowering those suffering from it and helping them to set boundaries to protect themselves from social media and others who abuse them. Educating the victims of mental health problems and having a more integrated or holistic approach when treating them, which will allow for educating their families and support systems.”
“Both MH and AOD issues went hand in hand for me. I think I would have started healing and growing much faster [if they had been treated in an integrated way].”
“It’s hard enough to open up to people and get a good connection. Only explaining yourself once would be fantastic.”
“In my experience it is difficult to see which one came first, but sitting in my shoes, it does not matter, it needs to be treated together, not sending me from mental health services to AOD services, back and forth. It needs to be treated holistically, and people need not give up on me because I have not ceased my drug use, or I relapse.”
“As soon as mental health services see AOD issues, they either refuse support or refer out. Mental health services do not do dual diagnosis well.”
“I had to go to so many different services and practitioners to find help. It took many years to and a lot of hard work and time by me to finally get on the right track.”
Reference: Barrett, E., et al. (2019). Lived experiences of Australians with mental health and AOD comorbidity and their perspectives on integrated treatment: Newparadigm Summer 2018 – 2019. NHMRC Centre of Research Excellence in Mental Health and Substance Use, National Drug and Alcohol Research Centre (NDARC), University of New South Wales, School of Medicine and Public Health, University of Newcastle, Australia. Pages 38 – 42.
The Story of Mr L
Methamphetamine (also known as “meth,” “speed,” “crank,” and “ice”) is a strong CNS stimulant that has become an increasingly popular illicit substance of abuse. It can be smoked, snorted, or injected. Use of the drug leads to experiences of prolonged euphoria, increased alertness and energy, and decreased food intake and sleep (Page 12).

CASE STUDY
“Mr. L” is a 55-year-old man with a past medical history of hypertension. He has a psychiatric history of posttraumatic stress disorder and an extensive substance use history, going back to his late 20s, of cocaine. He presented to the emergency department with the complaint of having worms under his skin. He was agitated, and his hands were covered in multiple excoriations. The patient’s vital signs were unremarkable except for his blood pressure, which was 182 mmHg/121 mmHg, and pulse, which was 110 beats per minute. He was breathing at a rate of 22 breaths per minute, with an oxygen saturation of 97% on room air. His urine drug screen was positive for cocaine and amphetamines.
The patient carried a plastic bag containing blood, which he claimed was full of worms he picked out with a scalpel. He also brought the scalpel, two knives, and a methamphetamine pipe in his personal bag. Medical staff was unable to visualize worms in the plastic bag or on the patient’s body. His physical examination was unremarkable except for excoriations on the dorsum of his hands. The patient was alert and oriented to person, place, and time, and he denied auditory, visual, and tactile hallucinations. Review of his medical record revealed that he had a presentation for a similar complaint three weeks prior and was prescribed pyrantel pamoate for a possible hookworm infestation. At that time, he related a history of having washed his dog in an inflatable pool, and the worms crawled from the dog and inside of him through his toenails, which were recently trimmed and bleeding.
A psychiatric consult was ordered due to the ongoing questionable complaint, not validated by others, as well as his history of mental illness, his high level of distress and agitation, and his drug screen results. The patient was ultimately admitted to an involuntary inpatient unit.
On initial encounter with the team, the patient attempted to point out worms under his skin. He picked off pieces of skin and scabs and screamed, “See these are the worms, this isn’t skin, I know skin!” He angrily denied all psychiatric review of system questions, was not prescribed any home medications, and remained focused on his dermatological complaint. On further interview, the patient revealed an extensive substance use history, particularly cocaine (smoked) and, most recently, methamphetamine (smoked). He reported that his first cocaine use was 26 years ago, with intermittent episodes of use, in much smaller amounts, throughout the years. A month prior to admission, he started smoking methamphetamine, an illicit substance he had not used in several years. He reported smoking, on average, 2 grams of methamphetamine every other day, with his most recent use on the day of his admission.
The patient was initially very distressed and would not cooperate with treatment until his dermatological condition was addressed. He was amenable to taking one dose of albendazole (400 mg) and initiating treatment with risperidone (2 mg twice daily). The following day, he was irritable and drowsy but maintained compliance with risperidone. The morning of the second day, he displayed complete resolution of his worm preoccupation. He was discharged on risperidone,
with a plan to taper off while being monitored for recurrence of symptoms. At discharge, the patient was calm, cooperative, and free of obsessional preoccupations. He was diagnosed with stimulant-induced perceptual disorder, with onset during intoxication.
Reference: Alec H. Fisher, B.A., Cornel N. Stanciu, M.D. Dartmouth. (2017). Amphetamine-Induced Delusional Infestation. American Journal of Psychiatry Residents Journal · December 2017. –Hitchcock Medical Center, USA. Page 12 – 13.
I Am Meth – Anonymous, 2011
“I destroy homes, I tear families apart; I take children, that’s just a start.
I’m more costly than diamonds, more precious than gold, the sorrow I bring is a sight to behold.
If you need me, remember I’m easily found; I live all around you-in schools, and in towns.
I live with the rich, I live with the poor, I live down the street, and maybe next door.
I’m made in a lab, but not like you think; I can be made under your kitchen sink;
In your child’s closet, and even in the woods; if this scares you to death, well it certainly should.
I have many names, but there’s one you know best-I’m sure you’ve heard of me, my name’s Crystal Meth.
My power is awesome, try me, you’ll see-but if you do you’ll never break free.
Just try me once, I might let you go, but try me twice and I’ll own your soul.
When I possess you, you’ll steal and you’ll lie. You do what you have to, just to get high.
The crimes you commit for my narcotic charms will be worth the pleasure you’ll feel in your arms.
You’ll lie to your mother, you’ll steal from your dad; when you see their tears, and you might feel sad.
But you’ll forget your morals and how you were raised; I’ll be your conscience; I’ll teach you my ways.
I take kids from parents, parents from kids; I turn people from God and separate friends.
I’ll take everything from you-your looks and your pride; I’ll be with you always, right by your side.
You’ll give up everything-down to the bone; and then realize you’re surely alone.
I’ll take and take till you have nothing more to give; when I’m finally done with you, you’ll be lucky to live.
If you try me, be warned, this is no game-if given the chance, I’ll drive you insane.
I’ll Ravish your body; I’ll control your mind. I’ll own you completely; your soul will be mine.
The nightmares I’ll give you while you’re lying in bed, the voices you’ll hear from inside your head.
The sweats: the shakes, the visions you’ll see-I want you to know these are all gifts from me.
But then it’s too late, and you know in your heart that you will always be mine and we’ll never part.
You’ll regret that you tired me; they always do, but you came to me, not I to you.
You knew this would happen, many times you were told, but you challenged my power and chose to be bold.
You could have said no and just walked away; if you could live that day over, now what would you say?
I’ll be your master; you’ll be my slave; I’ll even go with you when you go to your grave.
Now that you have met me, what will you do? Will you try me or not… it’s all up to you.
I can bring you more misery than words can tell; come take my hand, let me lead you to hell.”